Double Diabetes - Juggling Type 1 and Insulin Resistance
- Believe the hypo

- Oct 22, 2019
- 4 min read
What is double diabetes?
Managing diabetes is pain in the neck. It’s all consuming and we’re forced to balance out living the cleanest, most healthy life you can imagine with having some ‘treats’ now and again but the impact of these could be grim.
Basically, we can live a long and full life, but if we stray it may come back to bite us, and that’s not taking into consideration being genetically predisposed to anything nasty.
Staying positive in the face of such consistent adversity is a skill we must learn (and hold on to).
But there is a hidden, almost secretive type of diabetes that is rarely discussed and seldom declared. Double diabetes.
No, this isn’t simply diabetes but twice as bad.
This is when a person has type 1 diabetes and is also insulin resistant - a trait typical of type 2 diabetes.
Why is this noteworthy?
Type 1 diabetes (T1D) is categorised as an autoimmune disease. T1D’s insulin producing pancreatic cells, known as beta cells, are destroyed by the immune system and thus can no longer produce insulin. This is devastating as when we consume food, the bodies natural response is to secrete insulin to convert food into energy. When this doesn’t happen, it essentially turns the blood toxic impacting cells and organs.
Insulin resistance is when the bodies cells don’t respond normally to insulin and glucose builds up in the blood. This is not typical of T1D as it usually occurs in people who are obese. Although, T1’s have the capacity to develop insulin resistance just like anyone else.
What’s actually happening?
When we eat food (mostly carbohydrates) our body secretes insulin and metabolises food for energy and to feed our cells. The more carbohydrates we eat, the more insulin is produced.
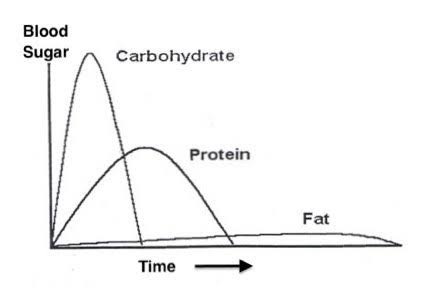
Quick note: The insulin response is different depending on what macronutrients we consume. Carbohydrates produce a rapid and large response: protein produces a slow and slight response and fat produces almost no insulin response, as depicted in the image below.
As you can see, the different foods we eat have a direct impact on the amounts of insulin produced. Over-time, consistently high insulin puts stress on the pancreas and leads to insulin resistance.
Depending on your genetics, you could be more carbohydrate intolerant than you realise - resulting in large blood sugar swings following the consumption of high carb foods.
Insulin is a fat storing hormone. As we eat more carbohydrates and produce more insulin, we won’t always burn off the glucose produced and this turns into fat and stored. The more fat we store, the more insulin is needed and in a cyclical pattern we become more resistant.
T1D’s are, in most cases, cautious of the amounts of carbohydrates we eat, so it’s natural to see a decreased incidence of insulin resistance. However, some T1’s may simply inject large amounts of insulin to cover carbohydrates consumed and this can lead to weight gain and insulin resistance.
Why is this problematic?
Insulin resistance is a major cause for concern by itself. It increases your risk for heart disease, stroke, cancer, cerebrovascular disease, fatty liver, osteoarthritis, hypertension, PCOS (polycystic ovary syndrome) and inflammation. Many scientists believe insulin resistance to be the major cause of modern disease.
Now add that to type 1 diabetes. A disease that is inherently difficult to manage and raises your risks of a host of metabolic diseases.
To put it another way; it’s like having a strong coffee when you already have diarrhoea. You’re making a bad situation much worse.
Diagnosis
If you have type 1 diabetes and you’re carrying extra weight, you may find your insulin requirements increasing. It’s important to not simply assume this is just part of being a diabetic - as our insulin requirements often do change - but this would rather be a sustained increase, often coinciding with body weight. Speak with your medical team frequently to discuss your insulin requirements and what may be affecting them.
How to reduce your risk
Simply put, lose weight.
Lower your carb intake. Increase your exercise levels and reduce highly processed foods from your diet.
A very effective strategy to lose weight, increase insulin sensitivity and help control blood sugars is the following:
a) Stop eating past 7pm.
b) Practice intermittent fasting - e.g. skip breakfast and have your first meal of the day at lunch. c) Remove processed foods - e.g. bread, pasta, cereal, chips, sweets, fast food and grain products. d) Get plenty of sleep. There is now a wealth of research proving low carb diets are more effective than moderate and high carb diets in improving insulin sensitivity, lowering body weight and controlling blood sugars. Both Diabetes UK and the American Diabetes Association both now endorse low carb and ketogenic diets.
Taking control
Putting on weight as we age is not an inevitability. The ‘middle age spread’ is not an inevitability. Increased insulin requirements is not an inevitability. Complications are not an inevitability, and double diabetes is not an inevitability.
Your health is in your hands... or rather, on your plate.
Nathan
Believe the hypo
www.believethehypo.com











This is an excellent blog Nathan. I have heard of this double diabetes before and your blog has been a real eye opener Thankyou 😀
This is very true of my experience.